Have your say on the Tech Plan for health and care
Consultation has concluded
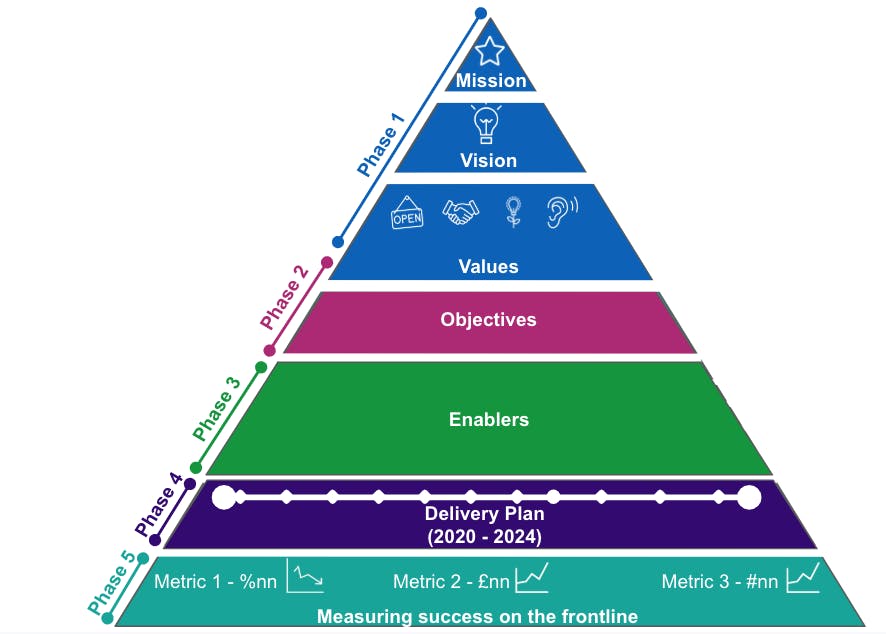
It is important that health and care services are designed around the needs of individuals and enabled by the right technology for the best experience and outcomes.
Our Tech Plan needs to be informed and co-produced by those on the front line, who are already bringing together people, technology and infrastructure to transform health and care.
Over the next few months we will use this website to collaborate with you on the Tech Plan. We will commit to:
- Working openly
- Be clear about what can and can’t be changed
- Tell you how we have taken account of your feedback
How to get involved
We want to involve as many people as possible to help us understand how we can best support the health and care system to deliver the ambition set out in the NHS Long Term Plan and the Department of Health’s Tech Vision, as well as the forthcoming NHS People Plan.
Through this platform, you can register to participate and share your views in the following ways:
- Comment on our vision - this is a working document and will be updated as we continue to engage on this. You do not need to register to see this but you do need to register to leave a comment.
- Register or sign in to share a case study - if you want to share how you have used tech to help transform services then we would love to hear from you. You can see the contributions others have made without signing in.
Over the next few months, new ways for you to get involved in the Tech Plan will be added here. By registering for the platform, we will be able to keep you updated as we develop the Tech Plan.
If you have any queries about this work or additional comments, please send these to us at techplan@nhsx.nhs.uk
Share a case study
Coronavirus (COVID-19):
As the health and care system responds to Coronavirus, we are pausing active engagement on this plan. In the meantime, you can still read the vision and mission document, and register for updates. 11/05/2020
The case studies below have been supplied by contributors and have not been checked for accuracy by NHSX.